Degenerative Disc Disease
Degenerative disc disease (DDD) is a condition where one or more discs in the back lose their strength and break down. Degenerative disc disease, despite the name, isn’t technically a disease. DDD is a progressive condition that can occur over time from wear and tear, or from injury.
The discs in your back are located in between the vertebrae of the spine. They act as cushions and shock absorbers. Discs help you stand up straight. And they also help you move through everyday motions, such as twisting around and bending over. Some people can have DDD without many symptoms, while others can suffer mild to extreme pain that can interfere with activities of daily living.
At Aptiva Health, we offer same-day and walk-in appointments for spine injuries and conditions to evaluate, diagnose, and make the appropriate referral for additional treatment based upon your specific spine injury or condition. We treat spine injuries and conditions in our Spine, Pain Management, General Medicine, Orthopedics, and Physical Therapy departments.
This graphic depicts the difference between a normal disc and a degenerated disc.
Symptoms and Causes
Disc degeneration may cause little to no symptoms, or could cause intense pain that could interfere with the performance of daily activities. Typically, DDD starts with damage to the spine, but in time, symptoms can affect other parts of the body. Symptoms can worsen as the degenerative process increases with age.
Common early symptoms include: pain and weakness in the back that can radiates to another area. If DDD takes place in the low back (lumbar spine) the symptoms and pain can radiate to the buttocks and upper thighs. In addition to pain, there may also be tingling, numbness, or both, in the legs or feet. If DDD takes place in the the neck (cervical spine) the pain may spread to the shoulder, arm, or hand.
DDD can also result in instability in the spine, leading to muscle spasms in the lower back or neck, as the body tries to stabilize the vertebrae. This condition can be quite painful.
causes
Intervertebral discs, also known as intervertebral fibrocartilage or spinal discs, provide the padding between the vertebrae of the spine. They have an elastic structure, made of fibrocartilage tissue. The outer part of the disc is known as the annulus fibrosus. It is tough and fibrous, and it consists of several overlapping layers. The inner core of the disc is the nucleus pulposus. It is soft and gelatinous. The intervertebral discs cushion when the spine moves or bears weight. They also help the spine to bend. As people age, repeated daily stresses on the spine and occasional injuries, including minor, unnoticed ones, can damage the discs in the back.
Changes include:
Loss of fluid: The intervertebral discs of a healthy young adult consist of up to 90 percent fluid. With age, the fluid content decreases, making the disc thinner. The distance between vertebrae becomes smaller, and it becomes less effective as a cushion, or shock-absorber.
Disc structure: Very small tears or cracks develop in the outer layer of the disc. The soft and gelatinous material in the inner part may seep through the cracks or tears, resulting in a bulging or rupturing disc. The disc may break into fragments.
When the vertebrae have less padding between them, the spine becomes less stable. To compensate, the body builds osteophytes (bone spurs) small bony projections that develop along the edge of bones. These projections can press against the spinal cord or spinal nerve roots. The development of osteophytes can undermine nerve function and cause pain.
Other problems include:
a breakdown of cartilage, the tissue that cushions the joints
a bulging disc, known as a herniated disc
a narrowing of the spinal canal, or spinal stenosis
These changes can affect the nerves, leading to pain, weakness, and numbness.
Diagnosis and Treatment
The most common imaging for DDD is MRI. X-rays of the spine are often added to complete the evaluation of the vertebra. Please note, however, that DDD is not always seen on plain x-rays. CT scan and myelogram were more commonly used before MRI, but now are infrequently ordered as initial diagnostic imaging, unless special circumstances exist that warrant their use. An electromyogram is also infrequently used to diagnose DDD.
X-ray: Application of radiation to produce a film or picture of a part of the body can show the structure of the vertebrae and the outline of the joints. X-rays of the spine are obtained to search for other potential causes of pain, i.e. tumors, infections, fractures, etc.
Computed tomography scan (CT or CAT scan): A diagnostic image created after a computer reads X-rays; can show the shape and size of the spinal canal, its contents and the structures around it.
Magnetic resonance imaging (MRI): A diagnostic test that produces 3D images of body structures using powerful magnets and computer technology; can show the spinal cord, nerve roots and surrounding areas as well as enlargement, degeneration and tumors.
Myelogram: An X-ray of the spinal canal following injection of a contrast material into the surrounding cerebrospinal fluid spaces; can show pressure on the spinal cord or nerves due to herniated discs, bone spurs or tumors.
Electromyogram and Nerve Conduction Studies (EMG/NCS): These tests measure the electrical impulse along nerve roots, peripheral nerves and muscle tissue. This will indicate whether there is ongoing nerve damage, if the nerves are in a state of healing from a past injury or whether there is another site of nerve compression. This test is infrequently ordered.
TREATMENT
Non-Surgical Treatments
The initial treatment for DDD is usually conservative and nonsurgical in the form of rest, medications, physical therapy, bracing, and injective therapy.
DDD is frequently treated with nonsteroidal anti-inflammatory medication, if the pain is only mild to moderate. The spine specialist may also recommend a course of physical therapy. A physical therapist will perform an in-depth evaluation, which, combined with the doctor's diagnosis, dictates a treatment specifically designed for patients with DDD. Therapy may include pelvic traction, gentle massage, ice and heat therapy, ultrasound, electrical muscle stimulation and stretching exercises. Pain medication and muscle relaxants may also be beneficial in conjunction with physical therapy. If pain and symptoms persist despite physical therapy. an epidural steroid injection may be performed utilizing a spinal needle under X-ray guidance (through the use of a c-arm) to direct the medication to the exact level of DDD for more moderate to severe symptoms.
Surgery
A doctor may recommend surgery if conservative treatment options, such as physical therapy and medications, do not reduce or end the pain altogether. Doctors discuss surgical options with patients to determine the proper procedure. As with any surgery, a patient's age, overall health and other issues are taken into consideration.
The benefits of surgery should be weighed carefully against its risks. Although a large percentage of patients with DDD report significant pain relief after surgery, there is no guarantee that surgery will help.
A patient may be considered a candidate for spinal surgery if:
Radicular pain limits normal activity or impairs quality of life
Progressive neurological deficits develop, such as leg weakness and/or numbness
Loss of normal bowel and bladder functions
Difficulty standing or walking
Medication and physical therapy are ineffective
The patient is in reasonably good health
Below are a list of common surgeries associated with DDD of the neck (cervical spine) and low back (lumbar spine):
lumbar spine surgery
Lumbar laminectomy, also called open decompression, is a surgical procedure performed to treat the symptoms of central spinal stenosis or narrowing of the spinal canal caused by DDD. The surgery involves removal of all or part of the lamina (posterior part of the vertebra) to provide more space for the compressed spinal cord and/or nerve roots.
Lumbar discectomy is a type of surgery to fix a disc in the lower back. This surgery uses smaller cuts (incisions) than an open lumbar discectomy. During a minimally invasive lumbar discectomy, an orthopedic surgeon takes out part of the damaged disc. This helps ease the pressure on the spinal cord. Your surgeon can use different methods to do this. With one method, your surgeon inserts a small tube through the skin on your back, between the vertebrae and into the space with the herniated disc. He or she then inserts tiny tools through the tube to remove a part of the disc. Or a laser may be used to remove part of the disc. Unlike an open lumbar discectomy, the surgeon makes only a very small skin incision and does not remove any bone or muscle.
Lumbar interbody fusion is a surgical technique that attempts to eliminate instability in the back. A MAS® TLIF achieves this by using a less invasive approach to fuse one or more vertebrae together to reduce their motion. In a MAS® TLIF procedure, rather than starting from the middle of the back and spreading the muscles to the sides like in a traditional back surgery, the MAS® TLIF approach starts off to one side of the back and splits (rather than cuts) the back muscles in one direction. This allows the surgeon to make a smaller incision with less muscle injury, which may result in less postoperative pain and a quicker recovery. This approach has proven to reduce blood loss, minimize scarring, reduce length of hospital stay, and allow for patients to recover quicker than conventional lumbar fusions. At Aptiva Health, our orthopedic spine surgeons specialize in the MAS® TLIF procedure.
cervical spine surgery
Cervical artificial disc replacement surgery (cervical arthroplasty) is a joint replacement procedure that involves inserting an artificial disc between the vertebrae to replace a natural spinal disc after it has been removed. This prosthetic device is designed to maintain motion in the treated vertebral segment. *Fun fact - Dr. Casnellie performed the first cervical disc arthroplasty in Kentucky.
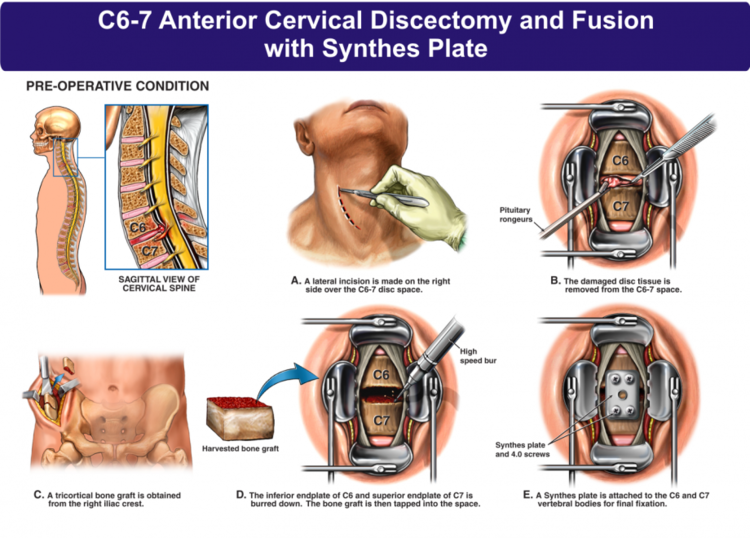
Anterior cervical discectomy and fusion (ACDF) is a surgery to remove a herniated or degenerative disc in the neck. An incision is made in the throat area to reach and remove the disc. A graft is inserted to fuse together the bones above and below the disc. ACDF surgery may be an option if physical therapy or medications fail to relieve your neck or arm pain caused by pinched nerves. Patients typically go home the same day. Find additional information and our post-operative instructions following ACDF here.