Headaches & Migraines
Although headaches and migraines both occur in the head, face, or upper neck, their severity, causes, and treatments can vary widely.
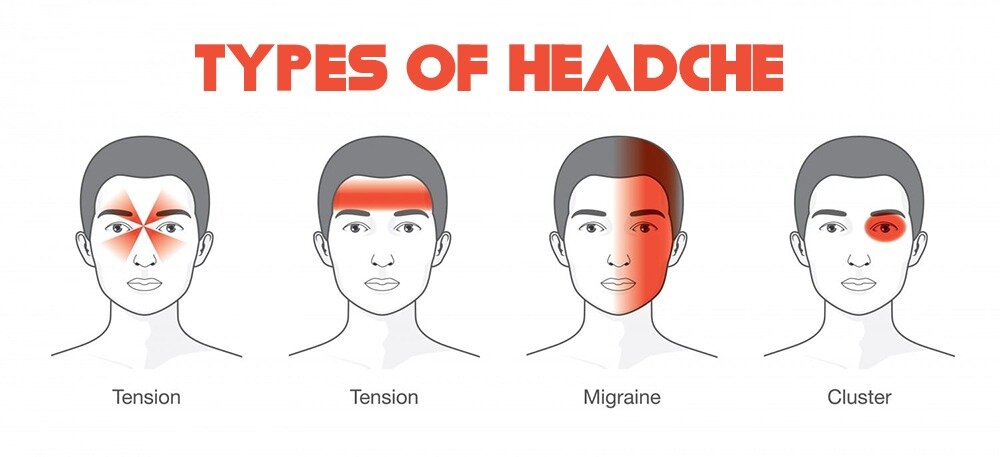
There are many different types of headaches, but most specialists break them into two main groups:
Primary Headaches: considered independent conditions that cause pain in the head, face, or neck. Examples of primary headaches include both migraines and tension headaches.
Secondary Headaches: stem from another medical conditions, such as an infection, stress, medication, or sickness.
Primary Headaches
Tension headaches
It is estimated that tension headaches impact around 42% of adults worldwide. Most commonly, tension headaches are described in a pattern that is “band-like” with intense pressure around the head. Tension headaches are broken down into episodic (occurring 10 to 15 days per month) or chronic (occur more often and may cause soreness).
There are many factors that have been linked to tension headaches, but a few are:
Stress
Lack of sleep
Hunger
Depression
Anxiety
Jaw clenching
Sleep apnea
Bending or straining the neck
Poor posture
Arthritis
cluster headaches
Typically cause severe pain on one side of the head, most often, behind the eye. These headaches come in clusters, meaning multiple headaches occur around the same time every day for several weeks. According to the National Institutes of Health (NIH), cluster headaches usually last 6 to 12 weeks. Cluster headaches tend to affect males more often than females.
Symptoms of cluster headaches include:
Pain behind the eye
Severe pain on one side of the head
Red and/or watery eyes
Sweating
Congestion
Restlessness
Agitation
Hemicrania
These are persistent headaches that fluctuate in severity, but typically affect the same side of the head. These headaches can be daily, or chronic.
Symptoms of hemicrania headaches include:
Sensitivity to light and/or sound
Nausea and/or vomiting
Sweating
Watery eyes
Redness or irritation of eyes
Congestion
Secondary Headaches
Illnesses and chronic medical conditions that affect the nervous system can cause secondary headaches.
Causes of secondary headaches include:
Sleep disorders
Brain tumors
Strokes
Withdrawal from medications or drugs
Head trauma or concussion
Inflammation
Seizures
Leaking spinal fluid
Physical deformations of the head, neck, or spine
Migraines
A migraine is a type of primary headache disorder that can cause severe pain and other symptoms that can range in severity. Migraines can cause intense, throbbing headaches that last anywhere from a few hours to several days. A migraine headache usually affects one side of the head, but some people experience pain on both sides.
A migraine episode can occur in four distinct phases, though not everyone experiences every phase.
Premonitory phase
Doctors also call the premonitory phase the preheadache or prodrome phase. It includes nonpainful symptoms that occur hours or days before the headache arrives.
Premonitory phase symptoms can include:
Unexplainable mood changes
Food cravings
Stiffness of the neck
Frequent yawning
Constipation or diarrhea
Sensitivity to light, sound, or smells
Aura phase
Auras refer to sensory disturbances that occur before or during a migraine attack. Auras can affect a person’s vision, touch, or speech.
Visual auras can cause the following symptoms in one or both eyes:
Flashing lights
Zig-zagging lines
Blurred vision
Blind spots that expand over time
Sensory auras cause numbness or tingling that starts in the arm and radiates to the face.
Motor auras affect a person’s ability to communicate and think clearly. Motor auras include:
Slurred or jumbled speech
Difficulty understanding what others say
Difficulty writing words or sentences
Trouble thinking clearly
Headache phase
Migraine headaches can range from mild to severe. People who have a severe migraine headache may need to seek emergency medical treatment.
Physical activity and exposure to light, sound, and smells worsen the pain. People can have migraine episodes without developing a headache, however.
Postdrome phase
The postdrome phase occurs after the headache subsides. People may feel exhausted, confused, or generally unwell during the postdrome phase.
This phase can last anywhere from a few hours or several days.
Diagnosis
A thorough physical examination with the General Medicine, Pain Management, or Physical Therapy Departments is the first step to diagnosing headache disorders. Your doctor will evaluate your signs and symptoms, review your medical history, and conduct a neurological examination.
IMAGING TESTS
Brain imaging may be recommended for some people with signs and symptoms such as severe headaches, seizures, repeated vomiting or symptoms that are becoming worse.
A cranial computerized tomography (CT) scan is the standard test in adults to assess the brain right after injury. A CT scan uses a series of X-rays to obtain cross-sectional images of your skull and brain.
Magnetic resonance imaging (MRI) may be used to identify changes in your brain or to diagnose complications or other considerations that could be causing recurrent headaches or migraines. An MRI uses powerful magnets and radio waves to produce detailed images of your brain.
Treatment at Aptiva Health
At Aptiva Health, our team of medical doctors and specialists will evaluate you to determine the best treatment plan dependent upon your individualized needs. Treatments can vary widely from conservative measures with simple over the counter medications to more invasive injective therapies aimed to block potential receptors or other issues that may be triggering headaches and migraines.
Over-the-counter medications
People can treat tension headaches and mild migraines with over-the-counter (OTC) medications. These include:
Pain relievers. These can include acetaminophen and nonsteroidal anti-inflammatory medications (NSAIDs), such as aspirin and ibuprofen.
Melatonin. A 2017 review cited findings from a number of randomized placebo-controlled trials that suggest melatonin may effectively prevent migraine and cluster headaches. The best dose may vary according to the condition, so a person should speak to a doctor about using this treatment.
Prescription medications
Moderate to severe migraine symptoms may not respond to OTC treatments. In this case, people may require prescription medications, including:
Antinausea medicines, such as beta-blockers
Triptans, such as almotriptan (Axert) or sumatriptan/naproxen (Treximet)
Ergot alkaloids, such as ergotamine (Ergomar)
People can also use prescription medication to prevent future migraines. Examples of these medications include:
Anti-seizure medications, such as topiramate (Topamax) or valproate (Depacon)
Antidepressants
Botulinum toxin A (Botox) injections
Nonmedication conservative prevention
Some lifestyle factors may also help prevent migraine episodes and some types of headache. These include:
Exercise regularly
Dietary changes that eliminate trigger foods
Relaxation techniques, such as mindful breathing and mediation
Therapeutic massage
injection therapies for headaches & migraines
Our Pain Management Team utilizes a variety of injection therapies to treat and help prevent headaches and migraines. These injection therapies include:
Trigger Point injections
Botox Injections