Sacroiliac (SI) Joint Dysfunction
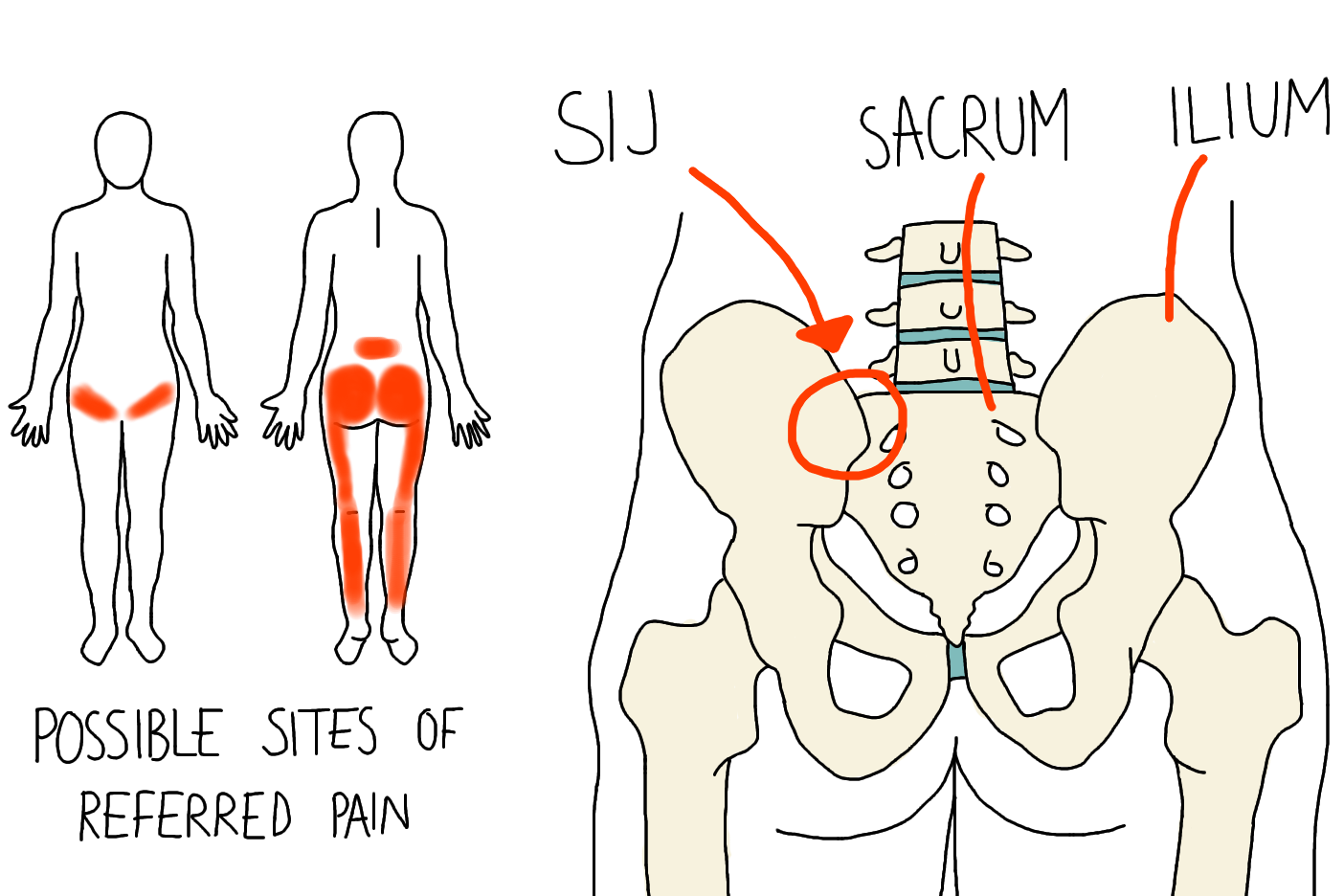
Pain from sacroiliac joint dysfunction can be felt anywhere in the lower back or spine, buttocks, pelvis, groin, or sometimes in the legs. Chronic SI joint pain symptoms can make it difficult to perform common daily tasks and can affect every aspect of a patient's life.
People with SI joint dysfunction can experience pain and impaired function. It's important to note that SI joint pain symptoms can be similar to those of other conditions of the lumbar spine, pelvis, and hip, and you will need an SI joint examination to properly diagnose the origin of the pain.
At Aptiva Health, we offer same-day and walk-in appointments for spine injuries and conditions to evaluate, diagnose, and make the appropriate referral for additional treatment based upon your specific spine injury or condition. We treat spine injuries and conditions in our Spine, Pain Management, General Medicine, Orthopedics, and Physical Therapy departments.
common si joint pain symptoms
Lower back pain (below L5)
Sensation in lower extremity; pain, numbness, tingling, weakness
Pelvis/buttock pain
Hip/groin pain
Feeling of leg instability (buckling, giving way)
Disturbed sleep patterns due to pain
Disturbed sitting patterns (unable to sit for long periods, sitting on one side)
Pain going from sitting to standing
what causes si joint pain?
Sacroiliac (SI) joint dysfunction and associated pain can be caused by a specific traumatic event (disruption) or can develop over time (degeneration).
Sacroiliac Trauma (common events that may cause SI joint disruption)
Motor vehicle accident
Fall on buttock
Lifting and/or twisting
Natural childbirth
Pregnancy (chronic low back pain during and/or after pregnancy is frequently referred to as pelvic girdle pain)
Sacroiliac Joint Degeneration (common causes)
Previous lumbar spine surgery (e.g., fusion of the lumbar vertebrae)
Stresses to the SI joint due to leg length differences, joint replacement, or scoliosis
Osteoarthritis
Previous iliac crest bone graft (ICBG)
Prior infection of the SI joint
Pain in the lower back and buttocks may be caused by the SI joint, hip, spine, or a combination of these structures. It is important that your doctor thoroughly evaluate ALL potential pain sources during a lower back pain exam in order to give you the proper diagnosis of your symptoms and prescribe the right path of treatment. Carefully review the typical symptoms of SI joint pain.
Treatment
If you have been diagnosed with SI joint dysfunction, which can lead to one or both of the SI joints becoming painful, your doctor will first recommend exploring conservative treatment options.
STEP 1 EARLY TREATMENTS
Medications may include:
Analgesics and NSAIDS
Opioid medications prescribed by a physician (opioids should be used only for a short period of time and under a physician’s supervision, as opioids can be addictive, aggravate depression, and have other side effects)
Anticonvulsants—prescribed drugs primarily used to treat seizures—may be useful in treating people with sciatica
Antidepressants such as tricyclics and serotonin, and norepinephrine reuptake inhibitors have been commonly prescribed for chronic low back pain (prescribed by a physician)
Self-management:
Hot or cold packs
Resuming normal activities as soon as possible may ease pain; bed rest is not recommended
Exercises that strengthen core or abdominal muscles may help to speed recovery from chronic low back pain. Always check first with a physician before starting an exercise program and to get a list of helpful exercises.
STEP 2 Additional CONSERVATIVE TREATMENT OPTIONS:
Transcutaneous electrical nerve stimulation (TENS) involves wearing a battery-powered device which places electrodes on the skin over the painful area that generate electrical impulses designed to block or modify the perception of pain
Physical therapy programs to strengthen core muscle groups that support the low back, improve mobility and flexibility, and promote proper positioning and posture are often used in combination with other interventions
Spinal manipulation and spinal mobilization are approaches in which doctors of chiropractic care use their hands to mobilize, adjust, massage, or stimulate the spine and the surrounding tissues. Manipulation involves a rapid movement over which the individual has no control; mobilization involves slower adjustment movements. The techniques may provide small to moderate short-term benefits in people with chronic low back pain but neither technique is appropriate when a person has an underlying medical cause for the back pain such as osteoporosis, spinal cord compression, or arthritis.
Traction involves the use of weights and pulleys to apply constant or intermittent force to gradually “pull” the skeletal structure into better alignment. Some people experience pain relief while in traction but the back pain tends to return once the traction is released.
Dry needling is moderately effective for chronic low back pain. It involves inserting thin needles into precise points throughout the body and stimulating them (by twisting or passing a low-voltage electrical current through them), which may cause the body to release naturally occurring painkilling chemicals such as endorphins, serotonin, and acetylcholine.
Behavioral approaches include:
Biofeedback involves attaching electrodes to the skin and using an electromyography machine that allows people to become aware of and control their breathing, muscle tension, heart rate, and skin temperature; people regulate their response to pain by using relaxation techniques
Cognitive therapy involves using relaxation and coping techniques to ease back pain
STEP 3 INJECTION THERAPY OPTIONS:
Interventional pain management injections to include:
SI Joint Injections. Sacroiliac (SI) joint pain is easily confused with back pain from the spine. Sometimes injecting the SI joint with lidocaine may help your doctor determine whether the SI joint is the source of your pain. If the joint is injected and your pain does not go away, it may be coming from a different source. During the procedure, a mixture of local anesthetic and steroid is injected into the SI joint. The local anesthetic will numb the area, and steroid may help lower the swelling. The steroid should reduce the pain and improve the motion in your hip or buttock.
Medial branch blocks injection used to determine if the facet joint is causing the patient's back pain. Facet joints are pairs of small joints between the vertebrae in the back of the spine.
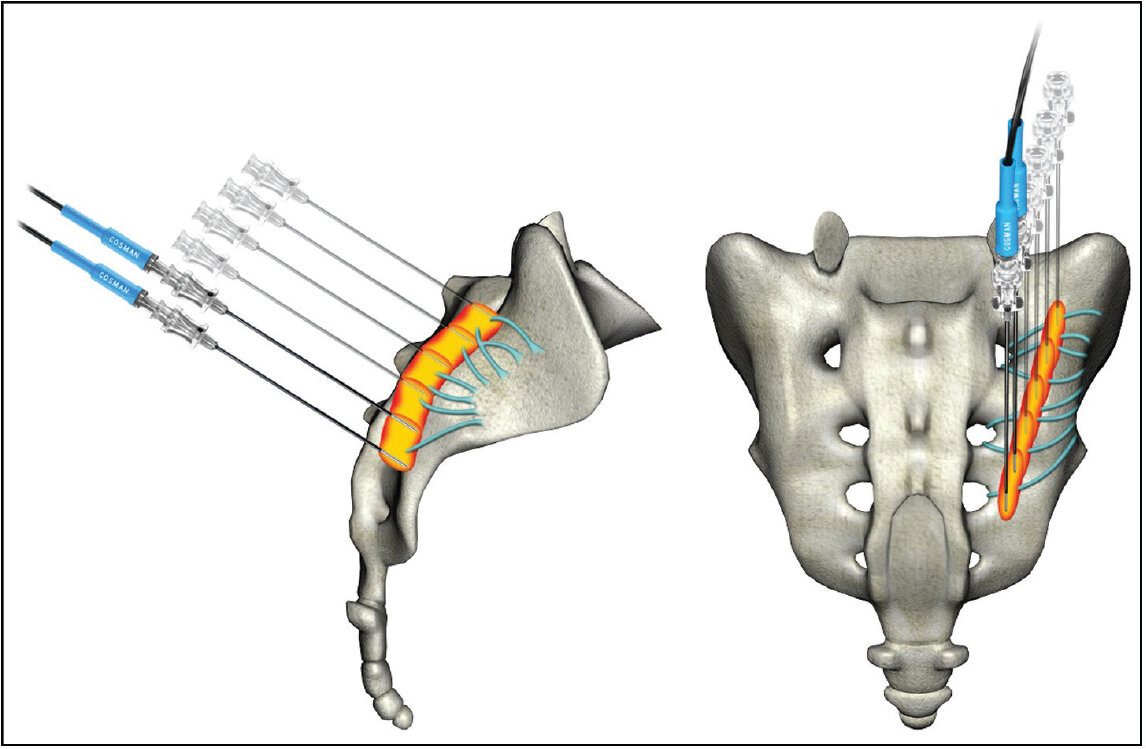
Radiofrequency ablation involves inserting a fine needle into the area causing the pain through which an electrode is passed and heated to destroy nerve fibers that carry pain signals to the brain. Also called a rhizotomy, the procedure can relieve pain for several months.
STEP 4 SURGERY
When other therapies fail, surgery (SI-joint fusion) may be considered to relieve pain caused by worsening pain and symptoms related to SI joint dysfunction.
SI-Joint fusion. The goal of this procedure is to completely eliminate movement at the sacroiliac joint by grafting together the ilium and sacrum. Sacroiliac fusion involves the use of implanted screws or rods, as well as a possible bone graft across the joint. Minimally-invasive procedures have been developed in recent years that improve outcomes in pain and disability, and reduce recovery time.
Hear from Lorie in the video below about her SI-joint fusion with Dr. Casnellie!
Studies show that the SI joint is a source of pain in 15-30% of patients with chronic low back pain. Does this include you?
For more information: